There are fairytales in science – and like the real, old-fashioned fairy tales they don’t always have a glossy finale, a kiss and a happily ever after.
There are tales in science that have a happy ending…
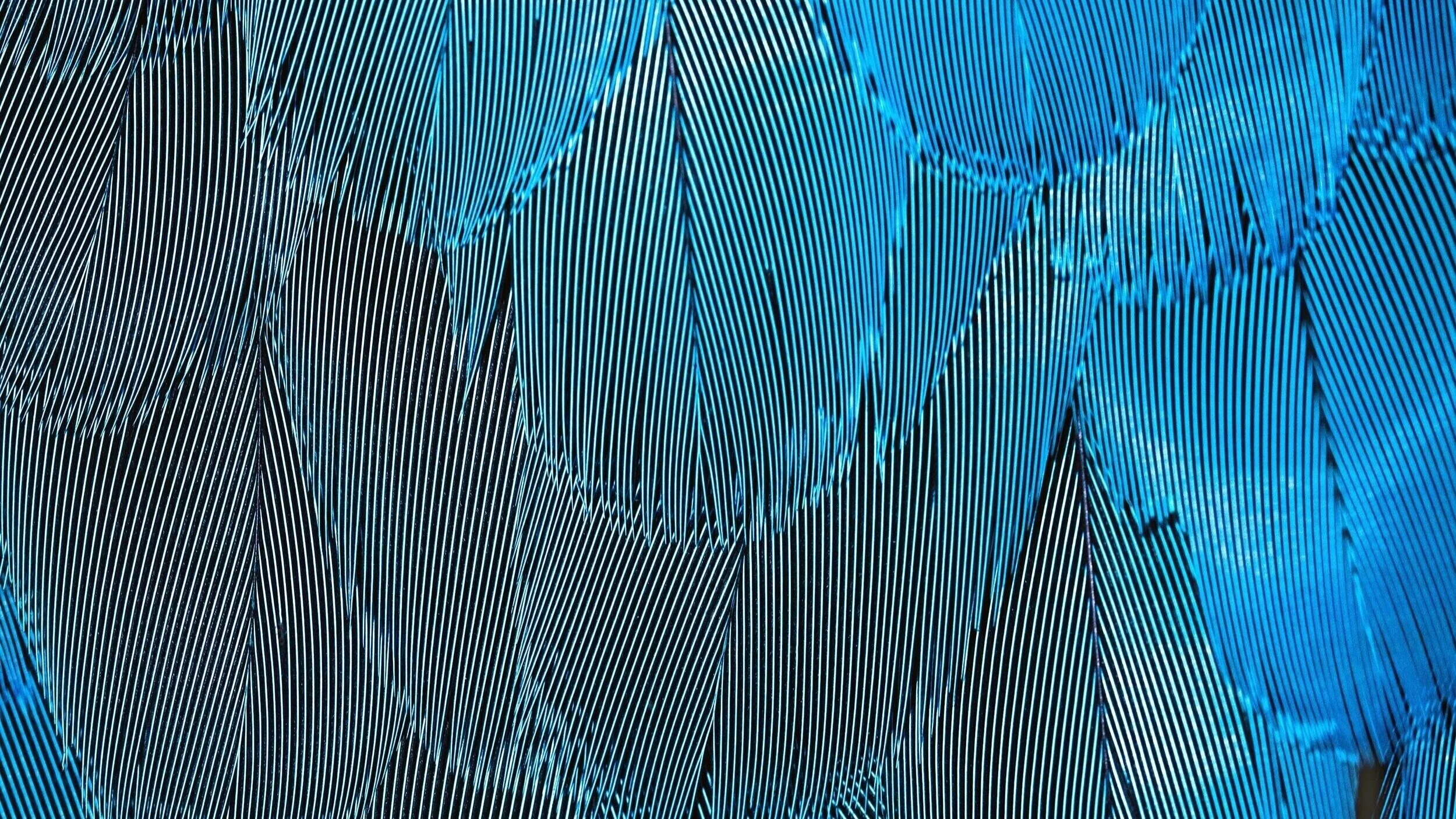
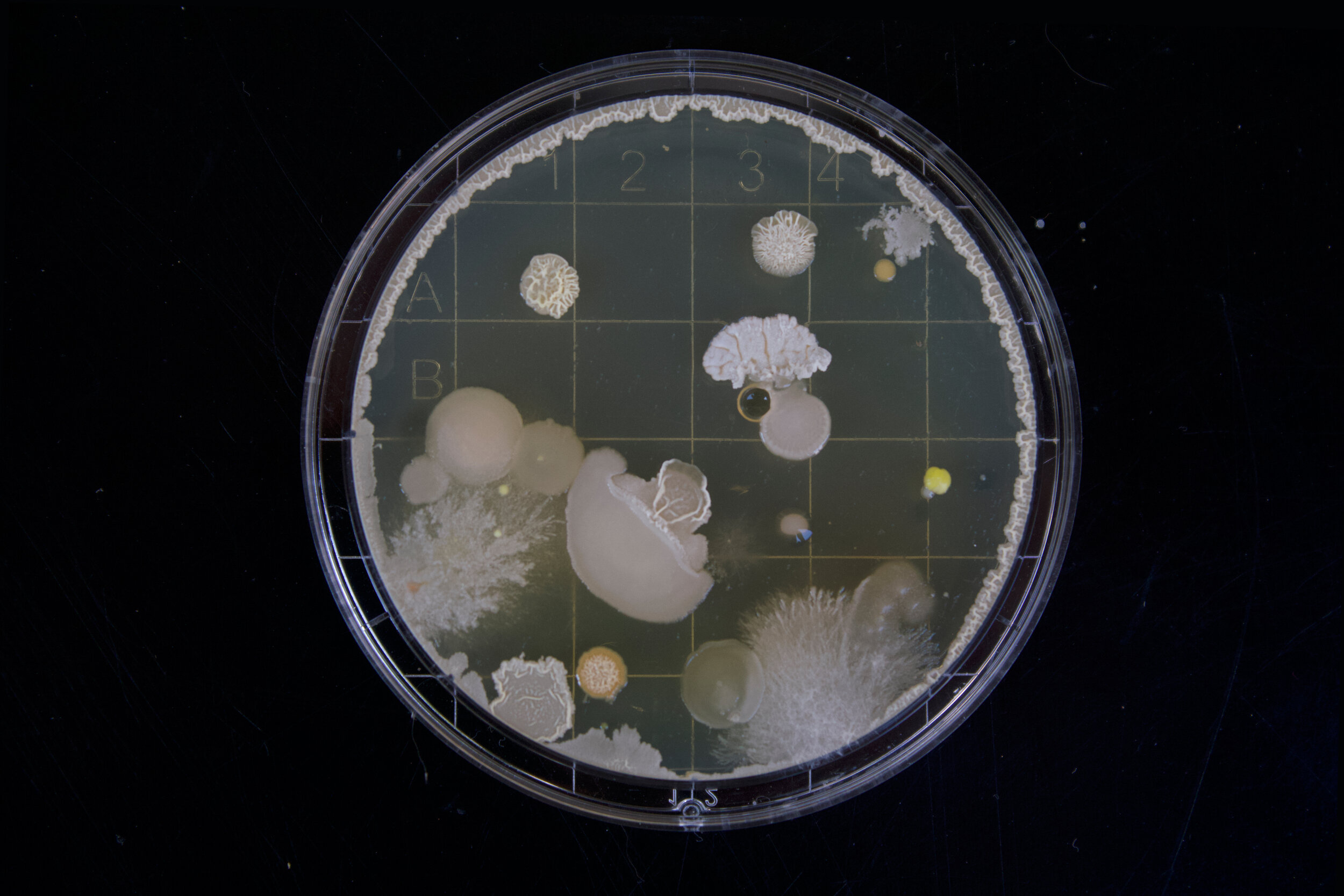
Those are tales of the moments of great discovery resulting from hard, year-long work or sometimes from pinch of serendipity – like the almost accidental discovery of Penicillin a drug that helped shaped the modern world by significantly contributing to the increase in life expectancy - from a meager 47 years at birth at the beginning of the 20th century to close to 80 years (in the US). A happy ending for the scientist Alexander Fleming (who’d forgotten to throw out his experimental plates before going on vacation), and a happy ending for humanity who suddenly had a new ally in the war against the microbial invaders.
There are darker tales too…
Dystopian scenarios introduce us to a world in which the scientific discovery feels like an already open Pandora’s box. One of the things that emerged from this box recently is gene editing, a technique that allows changing the genomes of species from mosquitos to humans in an unprecedentedly simple way, so simple in fact that you could do it at home with a preordered kit (if you are in a country which hasn’t banned the technology). A group of researchers who had discovered gene editing, the ones who had opened Pandora’s box, called for a moratorium on gene editing early on, before the public or politicians had caught wind of the potential dangers of the technology (we will read a lot more on gene editing in upcoming posts).
In equally dystopian scenarios the scientific discoveries that have protected us from hostile outside invaders that want to hijack our bodies – vaccines and antibiotics – fail due to human unwillingness to behave reasonably.
There are science tales that almost feel like horror stories…
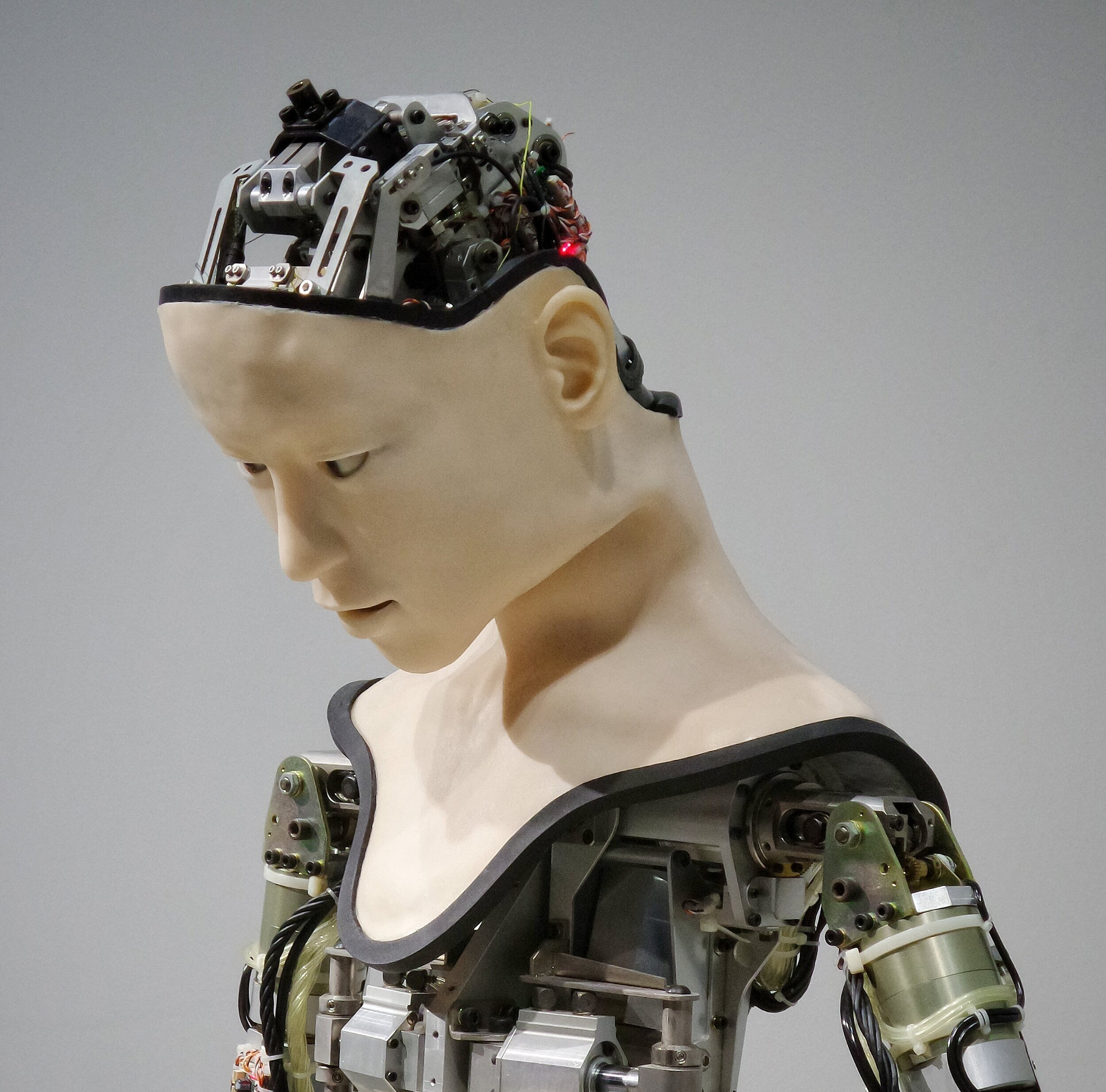
Maybe one of the most gruesome stories of modern science is that of lobotomies, in which a steel spike (the most prominent lobotomist Walter Freeman later changed to icepicks) is pushed into a person’s frontal brain to cure all kinds of symptoms from depression to schizophrenia, often leaving patients devoid of the symptoms, but also devoid of anything that resembled their former personality. Thousands and thousands of lobotomies were performed and the scientific community (or at least a part of it) was so convinced of the merits of lobotomy that its discoverer Egas Moniz, even received the Noble Prize for it.
Next Friday, we’ll start the science fairy tale series with one of the happy Science Tales – a true Snow-White story in which frozen people can be awoken with a kiss (though no dwarfs will be involved)…