When it comes to scientific discovery, there’s big news and there’s small news.
Lately, we’ve been drowning in the big COVID news: numbers, vaccines, mutants, and so on, leaving us just enough air to swim to the surface here and there to absorb the most recent success or failure of our favorite soccer team.
Still, there are science news important enough to penetrate the COVID bubble in our brains.
One such piece of news is Intellia’s first ever in vivo gene editing in humans - a milestone for a technology that can literally change humanity’s source code.
A permanent change
The US biotech Intellia was cofounded by Jennifer Doudna, one of a number of scientists who discovered the functionality of the bacterial CRISPR/CAS9 system through multiple discovery and one of two leading CRISPR scientists who were awarded the Noble Prize in 2020.
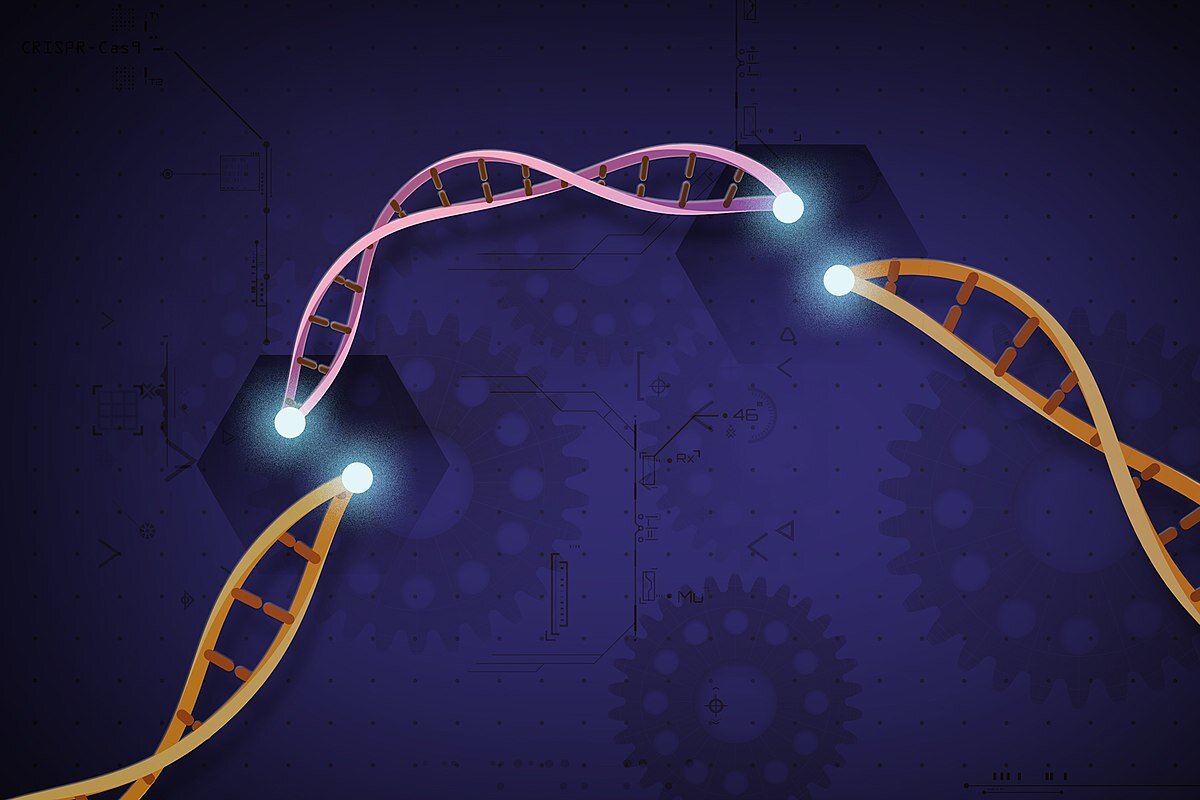
Gene therapy (the introduction of foreign genetic material into humans to cure disease) has been tested in patients for three decades though it was only in the 2010s that a few gene therapies saw approvals by the European and US regulatory agencies. CRISPR/CAS9 comes with a new level of precision that classical gene therapies don’t have. It allows making a change at a specific location in the genome, working with the cellular DNA repair machinery to excise and reknit DNA. With such a tool we can alter, remove or repair genes. If successful, CRISPR/CAS9 therapy could become a one-shot cure for many genetic diseases. It could also be a means to alter the human germline to select for desirable traits, like height, eye color, intelligence, or resistance against certain diseases. The latter was infamously attempted by Chinese researcher He Jiankui, now sentenced to three years in prison for trying to make human babies resistant to HIV...
While a number of researchers in biotechs and universities had used CRISPR-based gene therapy in patients, they performed the editing outside the body - a so-called ex vivo approach. Here, cells are extracted from the patient, genetically modified in the lab and then the altered cells are put back into the patient. Needless to say, ex vivo therapies are difficult, time consuming, prone to variability, and, most importantly – only work for diseases where it is possible to remove and add back cells into the patient. This is mainly true for blood diseases, such as Sickle cell anemia.
Intellia now performed a so-called in vivo approach, changing the gene directly in the patient. To be precise, they removed the gene which codes for the transthyretin protein, from the liver cells of patients, suffering from ATTR amyloidosis. This rare and fatal disease is caused by a mutation that causes buildups of misfolded transthyretin protein in the organs of the human body. A month after a single injection with Intellia’s CRISPR therapy, the researchers saw a decrease in protein levels of 80-96% in three patients.
On our way to Gattaca?
With CRISPR/CAS9 at our hands, will we soon be able to cure all genetic diseases including cancer? And if the method is so straightforward, how close are we to ordering our CRISPR kits for home use on Amazon and start improving our genomes, to turn ourselves in Gattaca-style beautiful and intelligent people?
Both scenarios are further away than it might appear at first glance, and not just because of ethical constraints. Changing the genome is not as easy as it sounds. While the technology appears ready (at least as ready as it gets, considering that it was discovered a mere decade ago), other factors challenge the use of CRISPR/ CAS9 just as much as classical gene therapies:
1. We don’t understand the human genome well enough to make the changes we want.
2. We don’t get the CRISPR/ CAS9 therapy (or any other gene therapy) where it needs to act.
Our lack of understanding is one of the major reasons of why, with all our fancy technology we in some respects haven’t moved a lot, have not cured cancer or Alzheimer’s or a myriad of other diseases. While we have some idea of deregulated genes in those diseases, we don’t fully understand how the disease manifestations are produced through the interplay of genes, epigenetics, and lifestyle factors. Trying to alter complex genetic networks will yield no result in the best case, and unintended consequences in worst.
There are diseases, however, where the removal of a single malfunctional gene, might be enough to halt their progression and potentially cure them. This is the case for numerous monogenic diseases, like the one that Intellia tackled - ATTR amyloidosis.
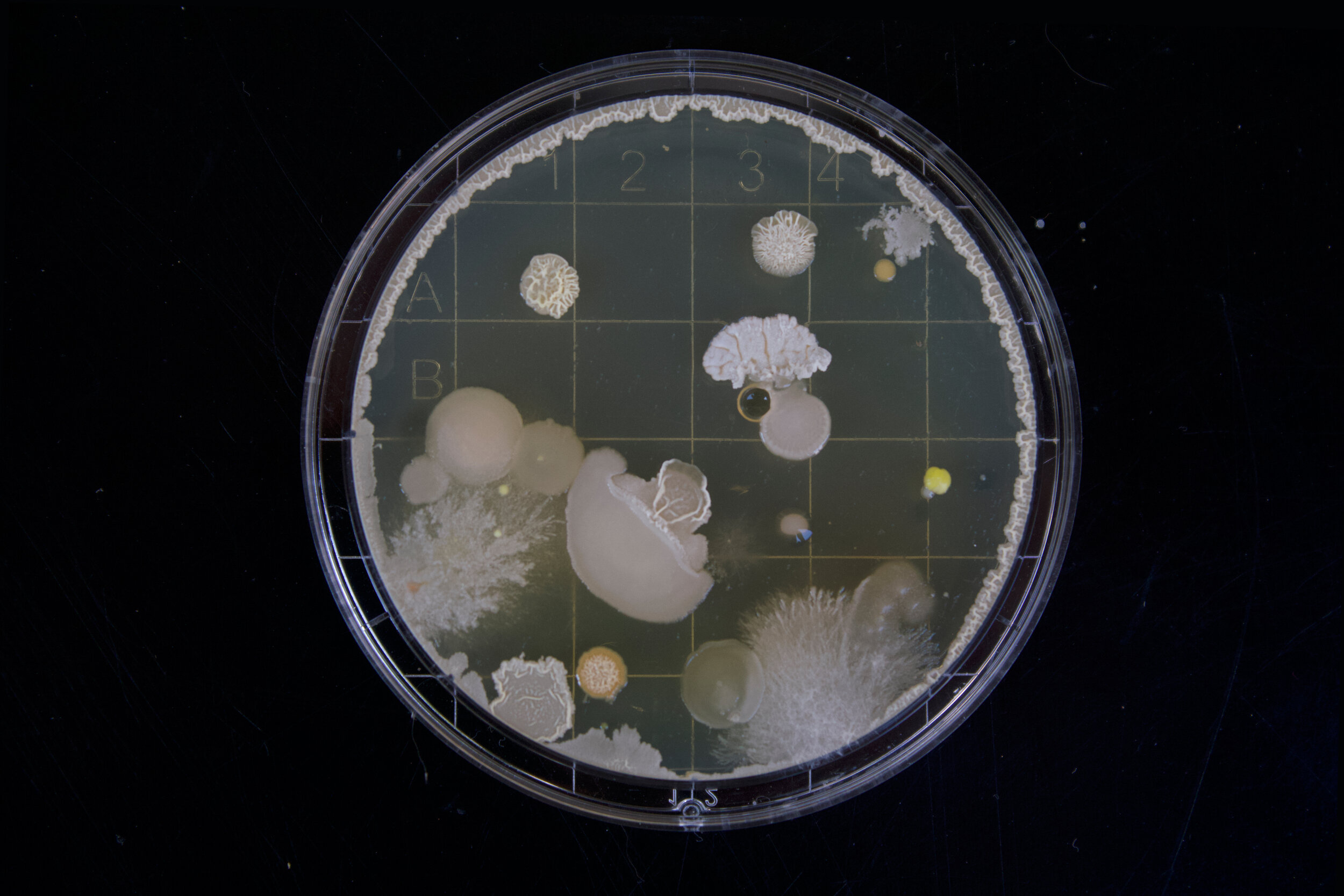
But even in cases, where the culprit gene is clear and we know where to put the DNA scalpel, we still need to be able to access the gene. Doing this is easier in a petri dish (as done in the ex vivo approaches for modifying blood cells or when manipulating human germ cells) than inside a human being. To be effective, enough of the gene therapy needs to reach the diseased tissue before the therapy is being diluted, neutralized or excreted. The human body is designed to get rid of foreign agents and not to neatly deliver them to the spot where the researcher wants them to act. Notably, one of the body’s major detoxifying organs is the liver, and most unwanted agents, be it an excess of alcohol, drugs or a gene therapies, will find their way there. For true in vivo approaches (meaning a therapy that is delivered systemically rather than locally, for example by direct injection into the eye), the liver is likely the easiest tissue to reach.
High stakes and low-hanging fruits
Researchers call those, comparably easy applications, the low-hanging fruit. While the groundbreaking example of Intellia would qualify as such as low-hanging fruit, it is an important proof of the technology, nonetheless. Does this mean it will work for more complex applications, such as multigenic diseases or difficult to reach tissues?
We don’t know yet.
But in science, problems are there to be solved and often serendipity is the scientist’s best friend. When Doudna and her peers were researching the bacterial immune system components, they hadn’t planned to hand humanity a tool that can rewrite its source code. During decades of hard work, they stumbled upon this particular application, and they were smart enough to understand what it could do and to contextualize its consequences.
Chances are, scientists will overcome the hurdles that CRISR is facing in more complex applications too. Maybe intentionally and maybe accidently, and probably through a combination of both. How soon, we can only guess.
But one thing is clear, we must acknowledge CRISPR/CAS9’s full potential with all its good and bad implications for humankind and prepare for the ethical challenges that it will bring.