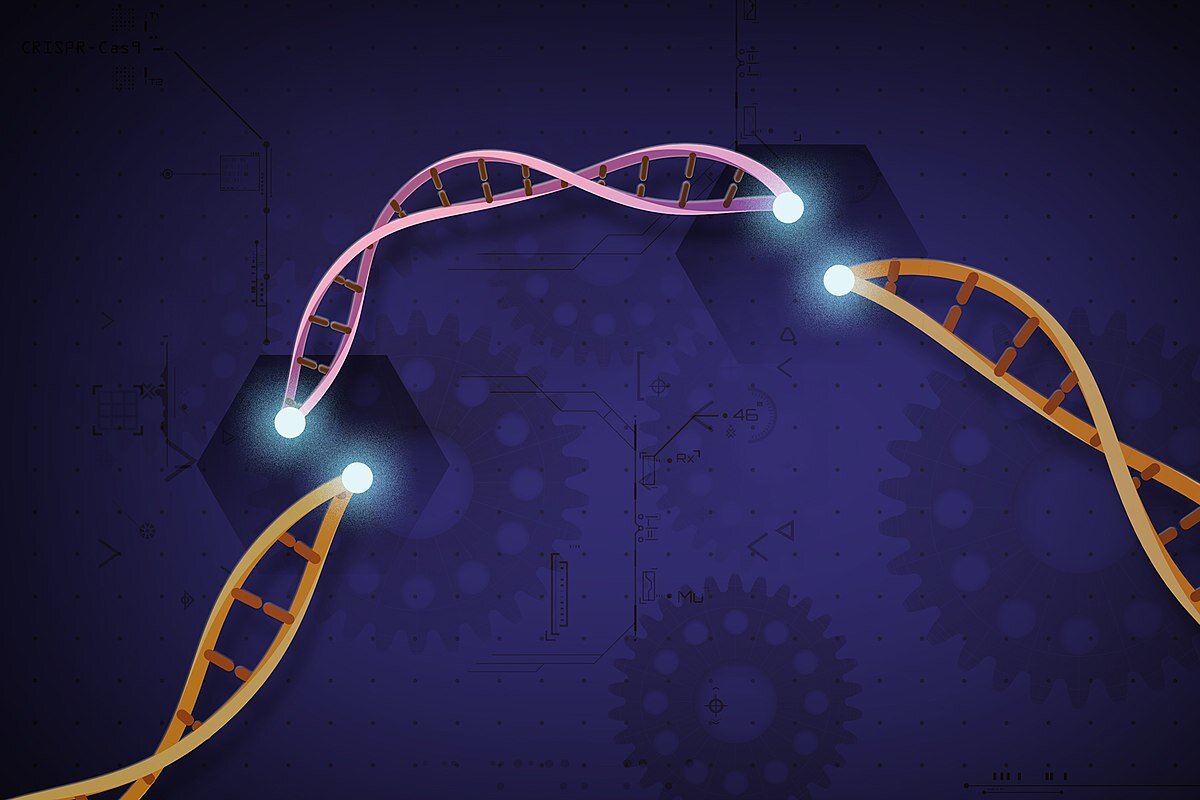
Both scenarios are further away than it might appear at first glance, and not just because of ethical constraints. Changing the genome is not as easy as it sounds. While the technology appears ready (at least as ready as it gets, considering that it was discovered a mere decade ago), other factors challenge the use of CRISPR/ CAS9 just as much as classical gene therapies:
1. We don’t understand the human genome well enough to make the changes we want.
2. We don’t get the CRISPR/ CAS9 therapy (or any other gene therapy) where it needs to act.
Our lack of understanding is one of the major reasons of why, with all our fancy technology we in some respects haven’t moved a lot, have not cured cancer or Alzheimer’s or a myriad of other diseases. While we have some idea of deregulated genes in those diseases, we don’t fully understand how the disease manifestations are produced through the interplay of genes, epigenetics, and lifestyle factors. Trying to alter complex genetic networks will yield no result in the best case, and unintended consequences in worst.
There are diseases, however, where the removal of a single malfunctional gene, might be enough to halt their progression and potentially cure them. This is the case for numerous monogenic diseases, like the one that Intellia tackled - ATTR amyloidosis.
But even in cases, where the culprit gene is clear and we know where to put the DNA scalpel, we still need to be able to access the gene. Doing this is easier in a petri dish (as done in the ex vivo approaches for modifying blood cells or when manipulating human germ cells) than inside a human being. To be effective, enough of the gene therapy needs to reach the diseased tissue before the therapy is being diluted, neutralized or excreted. The human body is designed to get rid of foreign agents and not to neatly deliver them to the spot where the researcher wants them to act. Notably, one of the body’s major detoxifying organs is the liver, and most unwanted agents, be it an excess of alcohol, drugs or a gene therapies, will find their way there. For true in vivo approaches (meaning a therapy that is delivered systemically rather than locally, for example by direct injection into the eye), the liver is likely the easiest tissue to reach.
High stakes and low-hanging fruits
Researchers call those, comparably easy applications, the low-hanging fruit. While the groundbreaking example of Intellia would qualify as such as low-hanging fruit, it is an important proof of the technology, nonetheless. Does this mean it will work for more complex applications, such as multigenic diseases or difficult to reach tissues?